Minimally invasive surgery and you — What’s changed?
OVER the past decade, there has been growing interest in minimally invasive surgery (MIS), and with good reason. These procedures offer smaller incisions, faster recovery, less pain, and fewer complications compared to traditional open surgery.
But what does that mean for the average Jamaican woman needing gynaecological surgery? And how accessible is it in the public health system today?
The answer is: more than you might think.
MIS in the public system — A quiet revolution
Minimally invasive gynaecological procedures are no longer confined to private hospitals. At May Pen Hospital, for instance, we perform both gynaecologic laparoscopy and hysteroscopy. These procedures include the treatment of ectopic pregnancies, removal of ovarian cysts, and diagnostic evaluation of the uterus.
We have seen improvements in infrastructure, which means that many of these procedures are available at no cost to the patient. However, there are still some limitations. Certain disposable items — like specialised trocars, uterine manipulators, or other specific laparoscopic instruments — are not consistently stocked in the public system. As a result, patients will sometimes need to purchase these from private suppliers.
Despite these hurdles, this marks a significant step forward in access to advanced surgical care for women in Jamaica.
Common myths about MIS — What you need to know
As more patients hear about MIS, I’ve noticed a few persistent myths that are worth addressing:
1) “Small cuts mean minor surgery.”
a) MIS still involves operating inside the abdomen, just with smaller incisions and less trauma. It’s not a “light” surgery, but it’s often safer and easier to recover from.
2) “MIS is only available in private hospitals.”
a) Not true. Gynaecologic laparoscopy and hysteroscopy are being done at May Pen and other public hospitals, with growing availability across the country.
3) “Recovery isn’t that different.”
a) Most women who undergo laparoscopy are able to go home within 24 hours, sometimes even the same day. They’re also back on their feet and returning to normal activities much faster than those who’ve had open surgery.
4) “It’s not as safe as traditional surgery.”
a) In trained hands, MIS is very safe — often with less blood loss, fewer infections, and lower complication rates.
5) “You can’t do real surgery through tiny holes.”
a) The technology has evolved. With high-definition cameras and precision instruments, we can safely treat a wide range of conditions with excellent outcomes. In fact, some complex dissections are actually easier to perform with laparoscopy than with open surgery.
Why this matters
Too often, I come across women who assume that “cutting the belly” is their only surgical option. Others delay care out of fear of long recovery times or being hospitalised for days. MIS offers a better alternative in many cases — one that reduces downtime and improves overall health outcomes.
Some of the blame lies with us, the professionals and the health system, to provide education to the public so they can make informed decisions.
We are committed to expanding these services, training staff, and improving access for more women in the public system.
If you or someone you know is facing gynecologic surgery, it’s worth asking: Is minimally invasive surgery an option for me?
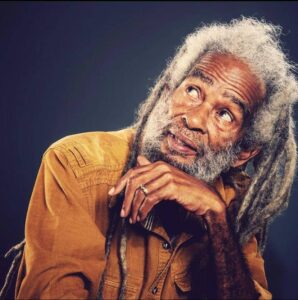
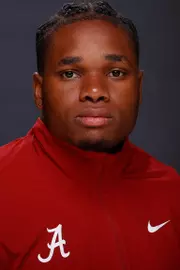
Dr Ryan Halsall, MBBS DMOG FACOG FMAS, is a consultant OBGYN | Minimally Invasive Surgeon. He operates ILAP Medical, Suite 2, 22 Windsor Avenue, Kingston.

Dr Ryan Halsall