One-stop cardiac care
JAMAICA now has its first heart hospital at the Heart Institute of the Caribbean (HIC) in St Andrew, which is dedicated to improving the outcome for patients with cardiovascular disease in Jamaica and the Caribbean region.
During a visit to the institution that has been transformed into a hospital solely responsible for cardiac care on Balmoral Avenue recently, the Jamaica Observer was given a tour of the facility by HIC’s founder and Chief Executive Officer Dr Ernest Madu.
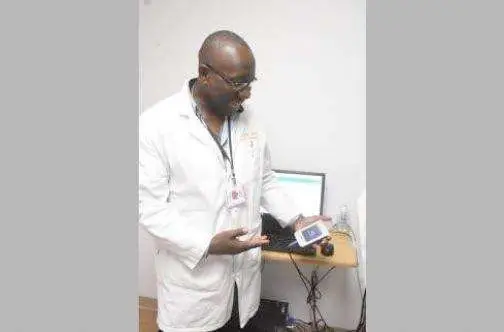
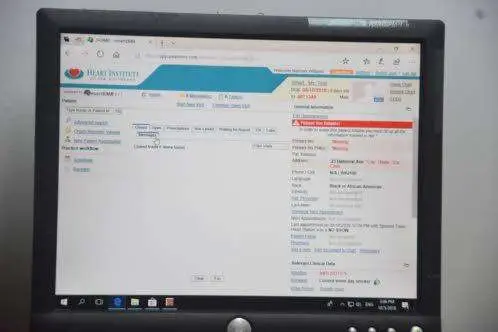
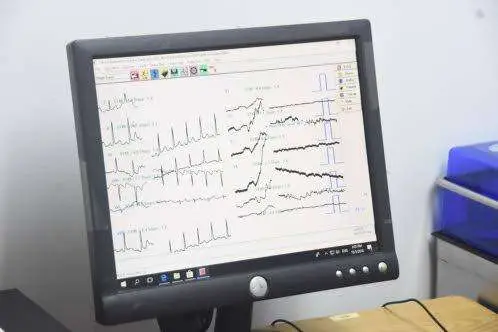
The 24-bed institution features a 24-hour cardiac ambulance service, an emergency room equipped with crash carts and defibrillators; state-of-the-art electrocardiogram machines the size of cellphones; password-protected electronic medical records, which allow for cooperation between doctors when documents are logged and reviewed by senior consultants from anywhere in the world; centrally monitored systems and specialised labs to include echocardiogram lab, nuclear cardiology lab, a catheterisation lab, a coronary care unit, a cardiac intensive care unit, and an operating theatre.
Other features of the cardiac hospital include tilt table testing — one of three such machines in Jamaica used to check fainting disorders; a vascular profile machine, the only one in Jamaica; a transoesophageal echocardiogram machine used to get a magnified view of the heart to see if there are infections, tears, or other complications; coronary angiograms and angioplasty; an electrophysiology system; exercise stress echocardiogram; carotid and vascular ultrasound; and pulmonary function tests.
The actual building which houses the hospital is designed with medical-grade floors for clinical practice, has antimicrobial walls, an air quality unit which has 15 air exchanges per hour and in the operating theatre 25 air exchanges per hour. Patients are centrally monitored through a computerised system at the nurses’ station, the walls and roofing are air and water tight and the operating theatre has UV lights that sanitise the area. Additionally, patient rooms have a nurse call button, single oxygen systems and beds that can calculate body weight, plus central music systems.
Another feature of the operating theatre is its waste anaesthetic gas disposal system to protect against cognitive impairment of physicians during surgery, and a camera operating in real time that allows surgeons across the world to assist during procedures.
The second floor of the institution houses a section called “Breath: A fresh approach to wellness”, which has a 23-hour observatory unit where patients not “fully admitted” are kept under observation. It is also equipped to deliver emergency dialysis if needed. The unit also has a gym which is used for physical therapy cardiac rehabilitation.
But being a private facility, what does this cost? Dr Madu explained that it all depends on the type of service one accesses; however, in general, care is estimated to be 50 per cent of what other private institutions charge.
Dr Madu also pointed out that in the 14 years of HIC’s operation, an open access to care model has been utilised.
“We ensure there is access first, then we look at cost. We do a means testing and we look at someone’s inability to pay versus their unwillingness to pay. Yearly we give away $120 to $130 million in free or subsidised care through the HIC Foundation. We have a membership programme which charges $25,000 per year and gives access to ECG and free consultations for 12 months, plus reduced costs of other services,” he shared.
HIC Foundation Executive Director Lisa D’Oyen added: “We are about supporting the mission of making care accessible regardless of ability to pay. We are bringing public health awareness to heart disease to the community. We have community days and access to services free or at a reduced cost.”
With regards to the need for a cardiac hospital locally, Dr Madu explained that the number one cause of death in Jamaica is cardiovascular diseases and the purpose of the hospital was to create a network or hub for cardiovascular care instead of having separate facilities.
“Cardiovascular care is a continuum. You have to have adequate oversight of the entire system to have the best care. If I put you in a hospital somewhere, I’m not there, I have no control over support staff or medication there. With this you realise care could be more optimal than you hope for. Doing this, we realised it was the right move. The patients were asking for it for years as when we send them elsewhere they don’t always get the type of care we think they deserve,” he explained.
Further, Dr Douglas Waldo, a team member at HIC, said the time was ripe for a full-fledged cardiac hospital in Jamaica.
“When I came to HIC many years ago, we did training from the ground up. I have done lot of mission work, but I came with an unrealistic idea of what I could do for the people of Kingston and Jamaica. We had to train nurses who didn’t have the same background as what we expected from cardiac nurses and it was not their fault. Now we have the capability. You usually hear that the number two cause of death is cancer, but what’s the number one? Heart disease. We have to address it,” Dr Waldo said.